PERI-IMPLANTITIS
Peri-implantitis is an inflammatory process that involves progressive bone loss and suppuration affecting the gum and bone surrounding an implant. It is associated with a bacterial infection that, unless successfully treated, leads to the eventual loss of the implant.
Frequently Asked Questions
1. What causes Peri-implantitis?
Peri-implantitis occurs as a result of a bacterial infection around an implant. The risk of such an occurrence is associated with many things, including a lack of oral hygiene around the implant, the way in which the implant and its restoration
were placed, and the overall health of the patient.
2. What are the risk factors associated with Peri-implantitis?
Any factors that increase bacterial colonization will increase a patient’s risks of
Peri-implantitis.
A) Generalized patient factors:
a. Poorly controlled Diabetes
b. Smoking (a significant risk)
c. Untreated Periodontitis [bone loss associated with gum disease]
d. A history of head and neck radiation therapy
e. Poor oral hygiene
B) Local implant/restoration factors:
a. An inability to clean the restoration on the implant
b. Excess cement associated with the final restoration
c. Loose, ill-fitting, or broken components
d. Poorly placed implants
3. How is Peri-implantitis diagnosed?
• Patient symptoms may include pain, mobility of the implant, and a bad taste.
However, in some cases there may be no symptoms.
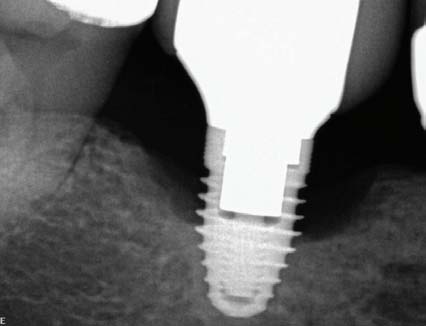
• Signs observed by your dentist or hygienist include suppuration and bleeding around the implant, progressive bone loss, and increasing pocket depths.



4. How is Peri-implantitis treated?
Non-surgical treatment: Carried out to reduce the extent of the defect and remove infected tissue. Usually results in improved local factors with no change in the resultant bone loss,
1. Mechanical cleaning around the implant and the localized placement of drugs
2. Laser and Photodynamic therapy Should the above prove unsuccessful, surgical treatment will be required.
Surgical treatment: Carried out to reverse the bone loss.
1. Open flap debridement to gain access, disinfect, and re-prepare the exposed surface of the implant.
2. Open flap debridement and disinfection with bone regeneration.
3. Laser therapy with or without flap access
5. What are the consequences if Peri-implantitis is not treated?
Both untreated and unsuccessfully treated peri-implantitis may lead to pain, a bad taste and increasing implant mobility. Eventually the implant, as well as teeth adjacent to the implant, may be lost. As well, significant bone loss around the implant jeopardizes the success of a new implant in the same site.



